Section title
In Washington, a debate took place about the rights of patients and the privileges given to physicians, hospitals, other medical providers, and insurers. H.R. 1215, named by its proponents as the “Protecting Access to Care Act of 2017,” promised to “improve patient access to health care services and provide improved medical care by reducing the excessive burden the liability system places on the health care delivery system,” while placing caps on the damages patients can recover, no matter how egregious the harm, among other harsh provisions. The White House's proposed budget sought to "reform the medical liability system" and purported to save money in this way.
These same promises were made in Texas 14 years ago when the state passed radical medical malpractice laws. These promises have not been kept, and patients, their families, and taxpayers have paid the price. Nearly a decade and a half in, the Texas experience reveals a trail of broken bodies and lives ended or altered forever – with insurers and the worst medical providers reaping the greatest rewards.
In our Constitutional Republic, we live by the principle that no person is above the law. But so-called “tort reform” laws violate that principle, giving privileges and immunities to a preferred class of people and industries, placing them beyond the reach of citizen jurors and judges. When the laws do not apply equally, wrongdoers escape accountability. And as the sections below show, when no one is accountable, no one is safe.
The Human Cost

Patient safety is in a state of crisis in America. This emergency is a story told day after day in waiting rooms and morgues across the country.
We entrust our medical care to professionals. Often, these professionals save lives. But sometimes this trust is violated and precious lives are ended or changed forever through carelessness, incompetence, or purposefully placing profits before people.
The latest analysis estimates over 250,000 Americans die each year due to medical errors, ranking it only behind heart disease and cancer as the third leading cause of death. In an attempt to put this staggering number in some perspective, that is the equivalent of having the entire population of a city the size of Lubbock, Texas wiped out each year. Or one 747 passenger jet, loaded to its highest capacity, crashing and disappearing into the ocean each day.
Faced with this crisis, one would think national leaders would be looking for ways to improve medical accountability and ensure patient safety. Instead, they are entertaining legislation, full of failed ideas, which will only make the problem worse. This prescription will inevitably lead to more death and destruction.
The Texas Experiment

Riding an electoral wave that saw the election of Rick Perry to his first full term as governor and a large class of impressionable freshman members in the Texas House of Representatives led by a hardline Speaker, the corporate immunity lobby tilled fertile soil in 2003. Emboldened after pushing through legal restrictions in 1995 and 1997, the lobby and their functionaries in the Legislature rammed through House Bill 4 in 2003, an omnibus package of restrictions that were sweeping in scope and unprecedented in their destructive effect on the rights and lives of everyday Texans.
Fourteen years later, patients in Texas continue to struggle with high cost, low access health care, wrongdoers are allowed to divert and evade responsibility for their actions, and our most vulnerable are most heavily penalized by limits on their individual legal rights.
Totaling 133 pages in length, HB 4 was a sprawling piece of legislation that upended and undercut myriad aspects of the Texas civil justice system. Among its most prominent provisions are those dealing with medical malpractice, nursing homes, and products liability. It has proven to be a failed experiment that ultimately sacrificed patients for profit.
Medical Malpractice
HB 4 restricts the rights of patients in numerous ways, including imposing a one-size-fits-all $250,000 cap on non-economic damages that effectively deprives many patients and their families of due process; allowing emergency room doctors to escape accountability for substandard care; and requiring patients to give pre-suit notice of any health care liability claims and file a detailed expert report within an arbitrary 120-day deadline (with case-killing penalties if they fail to do so).
Under Texas law, the value of one’s life is essentially reduced to the value of their paycheck.
The noneconomic damages cap, which is not indexed to inflation and thus worth less each year, hits those without wages and economic damages particularly hard, making even the most clear-cut malpractice cases on behalf of the elderly, the young, the disabled, and stay-at-home parents financially impossible to pursue for many given the high cost of retaining medical experts, which comprise the bulk of litigation expenses. The merits of one’s case are far outweighed by their socioeconomic status. Under Texas law, the value of one’s life is essentially reduced to the value of their paycheck. You are what you make. Life is cheapened and families are devalued. Instead of being a right possessed by all, what little justice remains becomes a privilege for the few.
A staggering and senseless number of Americans lose their lives to medical errors, making it all the more important to bear in mind that a mere 5.9% of physicians are responsible for 57.8% of all malpractice payments. Despite the extent of medical errors, researchers have demonstrated that as few as one out of every twenty-five patients with a negligent or preventable injury actually goes to the length of bringing a medical malpractice claim.
The reality of the situation in Texas was that from 1990 to 2002, the number of smaller paid claims declined sharply, and adjusted for the number of physicians or growth in real health care spending, the total number of paid claims and the number of large paid claims declined. However, these facts did not get in the way of the so-called tort “reformers,” who in their effort to carve up patient protections, cried that there was a “crisis” in medical malpractice claims as insurance premiums were ratcheted upward by carriers. Instead of improving the quality of medical care and investigating the accuracy of insurance premiums, safety was sacrificed and patients’ rights were eviscerated.
Because of our broken legal and regulatory systems, Texas has become a dumping ground for doctors with deeply distressing records
In this brave new world, a tiny state agency, the Office of Patient Protection, was supposed to serve as a counterbalance for patients, but it was smothered in the cradle before it could even represent any aggrieved patients. The Texas Medical Board, which nominally regulates physicians, does not have the will to consistently remove incompetent doctors from the practice, nor does it have a mechanism to compensate patients or adjust liability disputes between patients and doctors. Because of our broken legal and regulatory systems, Texas has become a dumping ground for doctors with deeply distressing records like Pamela Johnson, Stefan Konasiewicz, and Christopher Duntsch, the neurosurgeon whose reign of terror was finally ended by the criminal justice system when he was sentenced to life in prison for his butchery. Dr. Donald Okechukwu Ozumba, a McKinney surgeon, currently faces two charges of sexual assault allegedly committed against his patients.
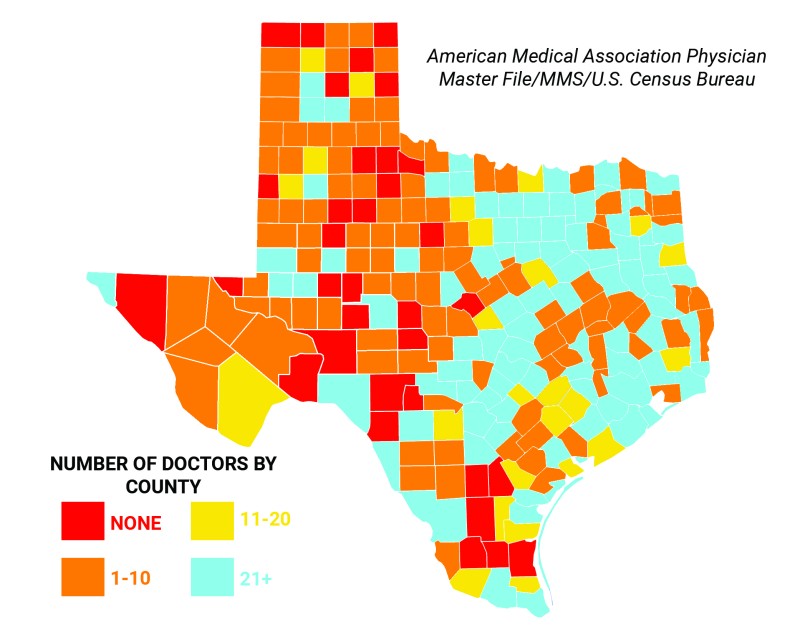
Heat map of doctors by county in Texas. 63 Texas counties have no hospital, 27 counties have no primary care physicians, and 16 counties have only one such doctor.
Restrictions on patients’ rights were sold with lofty promises about access to care, such as then-Governor Perry’s statement that HB 4 would “protect patient access to quality health care.” However, this rhetoric does not reflect reality. Texas ranks 1st in the percent of the population without health insurance. Texas has fewer physicians per 100,000 working-age people when compared to other large states like California, New York, Florida, and Illinois. Rick Perry’s claims about Texas gaining doctors due to “tort reform” have been thoroughly investigated and determined to be outright false by the Pulitzer Prize-winning PolitiFact.
Rural communities remain grossly understaffed and underserved, with 63 Texas counties having no hospital, 27 counties having no primary care physicians, and 16 counties having only one such doctor. Roughly half of this 268,000 square mile state is covered by trauma centers in just two cities: El Paso and Lubbock. According to one recent study of the physician workforce in Texas, 35 Texas counties have no physicians of any kind, 80 Texas counties have five or fewer physicians, 147 Texas counties have no obstetrician/gynecologist, 185 Texas counties have no general psychiatrist, and 158 Texas counties have no general surgeon.
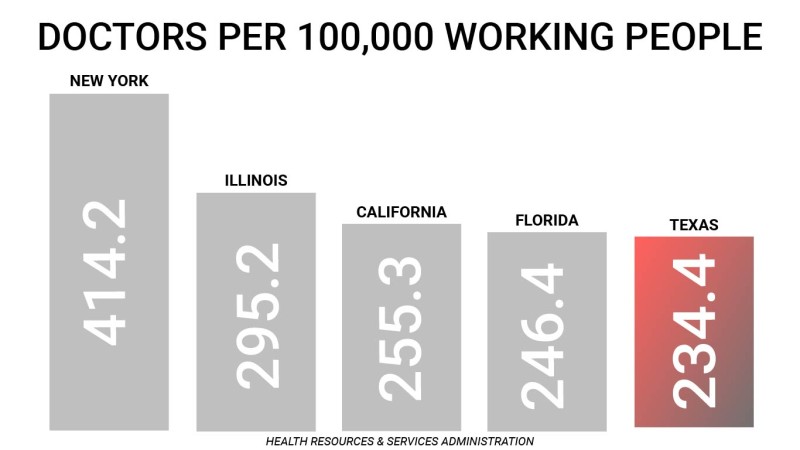
In a 2008 academic study on the impact of HB 4 on physician supply, researchers concluded that “Texas was not losing physicians before HB 4 took effect,” “the data do not yet support claims of dramatic improvements in patient access to physicians,” and “tort reform had limited impact on the number of DPC [direct patient care] physicians, including DPC specialists.” In follow-up research published in 2012 that looked at a longer trend of physician supply data, the same scholars concluded: “Physician supply was not stunted prior to reform, and it did not measurably improve after reform. This is true whether one looks at the number of patient care physicians in Texas, the number of Texas physicians in high-malpractice-risk specialties, or the number of physicians per capita in Texas relative to other states.” Today, Texas ranks 47th in the nation in active primary care physicians (PCPs) per 100,000 population.
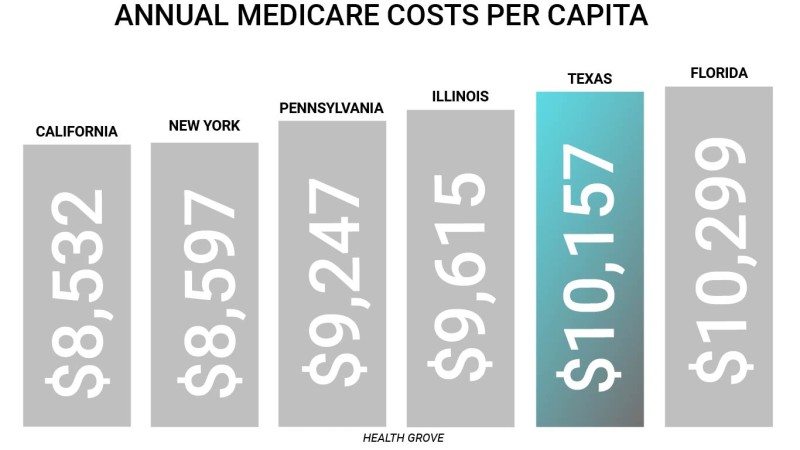
Furthermore, health care costs for both families and taxpayers continue to rise. Annual health insurance premiums paid by employees (not including employer contributions) for Texas families have increased from $1,759 in 2000 to $5,409 in 2015 – a whopping 207.5% increase in out-of-pocket premiums paid by Texas workers. Thirty-one percent of Texans are underinsured compared with 19 percent of Californians and 22 percent of New Yorkers. The share of insured adults in Texas with high deductibles relative to income exceeds the national average at 15 percent, while California and New York have considerably lower shares at 6 percent. Meanwhile, Texas outpaces other large states like California, New York, Illinois, and Pennsylvania when it comes to Medicare spending and usage on a standardized, risk-adjusted, per capita cost basis.
Creating special privileges under the laws for doctors and hospitals has not reduced costs by leading to fewer “defensive medicine” practices. A recent study in the esteemed New England Journal of Medicine found no reduction in “defensive medicine” practices when it looked at the experiences of three states – Texas, Georgia, and South Carolina – which have heightened bars for recovery against emergency care providers.
Physician supply was not stunted prior to reform, and it did not measurably improve after reform
The authors of the study concluded: “We did not find evidence that these reforms decreased practice intensity, as measured by the rate of the use of advanced imaging, by the rate of hospital admission, or in two of three cases, by average charges. Although there was a small reduction in charges in one of the three states (Georgia), our results in aggregate suggest that these strongly protective laws caused little (if any) change in practice intensity among physicians caring for Medicare patients in emergency departments.” Stated plainly, the physicians in these states are still over-practicing medicine despite the passage of laws that restrict patients’ legal rights.
These so-called “tort reform” laws haven’t increased access or contained costs – they’ve only restricted rights. Texas’ medical crisis for patients has only been exacerbated by a crisis in its judicial system, as many patients have access to neither a doctor in the event of illness nor a courtroom in the event of suffering a preventable injury. The biggest beneficiaries of this rigged system are the professional liability insurers who are able to routinely collect premiums for malpractice policies that they will rarely have to pay out on.

Nursing Homes
Nursing homes should exercise the most attentive care while helping our most vulnerable citizens live out their final years with dignity. Residents of nursing homes, and their families, are counting on them to provide a professional and caring environment for those who can not care for themselves. It is in the name, after all. These should be homes, not profit-seeking warehouses.
Given these stakes, it is shocking to comprehend that nursing homes were given the state’s seal of approval to “go bare” and forgo liability insurance altogether during the 2003 legislative session. You must have insurance to drive a car, but you are not required to have insurance to operate a nursing home in Texas. This means these facilities have been authorized to operate irresponsibly – with de facto immunity – as no victim’s attorney will be able to incur the expense of prosecuting their negligence without the ability to recover from the wrongdoer. You can have a case, but without the means to recover, you will not receive justice. In addition, the Texas Legislature wrote nursing homes into HB 4 and made it exceptionally difficult to admit records of their administrative violations and penalties into evidence during trial. This serves no purpose other than to thwart transparency and shield wrongdoers from accountability.
51% of Texas nursing homes are one or two star rated
It should come as no surprise, then, that given the ability to operate without any real accountability, nursing homes in Texas have cut corners and endangered patients, ranking as the worst in the nation with the highest percentage of one- and two-star facilities and over half of all facilities ranking “below average” or “much below average.” This has prompted one expert to note that “you don’t want to be old” in Texas. For-profit nursing homes tend to have lower ratings than non-profit nursing homes. Texas is tied only with Oklahoma for the highest percentage of for-profit nursing homes, leading the nation with 86%.
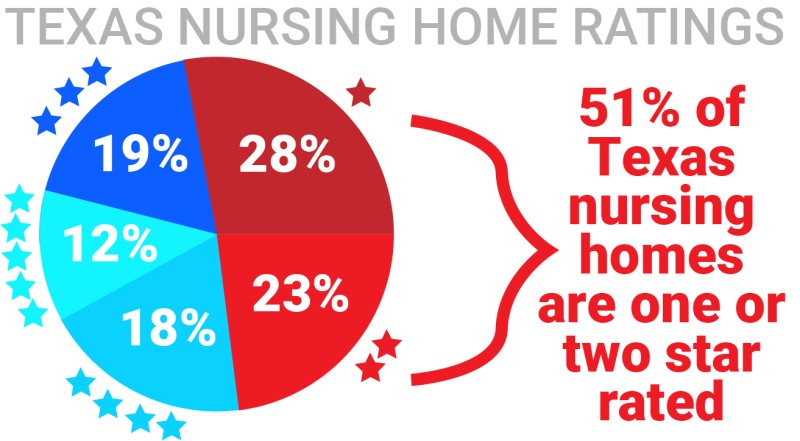
51% of Texas nursing homes are one or two star rated
A recent study by AARP Texas entitled "Intolerable Care" found Texas nursing homes commit serious licensing violations, the state does not consistently take enforcement action against them, and the state also fails to assess meaningful sanctions against serious and repeat offenders. The study determined: "Many nursing homes have serious and repeat violations but are not sanctioned by the state. In fiscal years 2014 and 2015, 328 of the state’s 1,200+ nursing facilities accounted for 94 percent of all serious violations. Of those 328 facilities, the state collected fines from only 22 of them."
Through deliberate public policy choices such as these, the Texas political leadership has demonstrated their belief that life, in the end, means little.
Texas courts must defer to Federal agencies in many state products liability actions
Products Liability
Section 6 of proposed H.R. 1215 reads: “A health care provider who prescribes, or who dispenses pursuant to a prescription, a medical product approved, licensed, or cleared by the Food and Drug Administration shall not be named as a party to a product liability lawsuit involving such product and shall not be liable to a claimant in a class action lawsuit against the manufacturer, distributor, or seller of such product.” A similar FDA shield has been used since 2003 in Texas.
HB 4 directed Texas courts to defer to federal agencies in many state products liability actions, strange for a state that is fiercely independent and that resists federal intervention at virtually every turn. For actions alleging inadequate warnings regarding pharmaceuticals, a rebuttable presumption is created in favor of defendants if the warnings that accompanied the product were approved by the United States Food and Drug Administration (i.e., the “FDA defense”). And in other products liability actions concerning the formulation, labeling, or design of a product, a similar rebuttable presumption (i.e., a legal conclusion that is taken as true unless proven otherwise) is created for product manufacturers or sellers who show that they complied with federal regulations.
At base, these reforms act to deprive state judges and juries of their ability to determine whether a product is unsafe, ceding this authority instead to unelected, unaccountable federal bureaucrats in agencies that have often been purposefully understaffed and underfunded, constrained in their authority, and are otherwise subject to influence by the industries that they are supposed to regulate.
CONCLUSION: Tort "Reform" Costs Lives
As Texas – and the nation – looks back at the impact of HB 4 over the course of the last 14 years, it is abundantly clear that its so-called “reforms” were not designed to help individual Texans. You do not help people by taking away their rights and giving special privileges to others. Access to care and quality of care has not improved for many Texans, as the state lags behind others. Costs have not come down for patients. Dangerous doctors have set up shop in the state, and other doctors continue to practice defensive medicine despite the special privileges they have been given.
In the end, the story of the 2003 legislation is the violence it has done to our system of justice. It is nothing less than a Texas tragedy. Through HB 4 and its progeny, our state has traded meaningful, public accountability for immunity, leaving untold numbers of Texas families to bear the financial, physical, and emotional costs of needless harm so wrongdoers and their insurance cohorts can avoid legal responsibility. The legislation has undoubtedly maximized profit while also maximizing misery.
The nation can avoid Texas’ mistakes by rejecting the false promises of the insurers and providers and recognizing H.R. 1215 for what it is: special interest legislation that will benefit a very few at the expense of the rest of us. This is a tragedy that must be avoided because untold millions of lives across this country are at stake.
Resources